Oesophageal and gastric surgery
Reflux surgery – Oesophageal and stomach surgery – Oesophageal cancer (heartburn, stomach burn, acid regurgitation, reflux, Barrett’s, oesophagus, oesophageal cancer)
“I have been interested in the organs of the upper gastrointestinal tract (upper GI) for 25 years.” Dr. Jörg Zehetner, Professor
These include the oesophagus, stomach and small intestine.
Many people (between 20-30% in the western world) suffer from occasional reflux (regurgitation of gastric juice into the oesophagus).
This leads to chronic discomfort and in the long run can lead to changes in the mucous membrane, and subsequently to cancer.
Especially for patients who have been taking acid blockers (PPI) for a long time, the question arises: When was the last gastroscopy? Has a functional diagnosis of the oesophagus been carried out? Have you ever had a conversation with a surgeon?
“If you are taking acid blockers but still have symptoms, then you should register for a consultation about the new methods of modern reflux treatment in one of our Swiss1Chirurgie clinics.”
Jörg Zehetner, MD, Professor (USC), MMM, FACS, FEBS
After years in Switzerland and Austria, Dr Jörg Zehetner spent a total of 7 years at the world’s most renowned clinic for reflux disease and oesophageal cancer from 2008-2015, and Dr Tom DeMeester was his mentor. No one in the world has published more papers on reflux than he has. Other mentors were Dr Christian Klaiber (father of laparoscopic surgery in Switzerland) in Switzerland, Prof Wolfgang Wayand (father of laparoscopic surgery in Austria) and Dr Jan Danis (inventor of the Danis stent for oesophageal variceal bleeding) in Austria. Other mentors in the USA were Dr Steve DeMeester, Dr Namir Katkhouda and Dr John Lipham.
Keyword REFLUX TREATMENT
Dr Jörg Zehetner has been in Bern since July 2015, initially as a practice partner of Dr Steffen at Schänzlihalde 1 in Bern. In July 2017, he took over the clinic and established Swiss1Chirurgie AG with locations in Bern, Solothurn and Valais.
He is the only surgeon to offer all standard reflux surgery procedures.
These include laparoscopic hiatal hernia surgery with Nissen or Toupet fundoplication, i.e. complete or partial gastric sleeve.
Of the modern procedures, Dr. Jörg Zehetner has learned all possible procedures in Switzerland and has the latest technology at his disposal. In laparoscopic reflux surgery with the Linx Reflux Management System (the only centre in the canton of Bern), Dr Jörg Zehetner has the most experience of any surgeon in Switzerland. He has now operated on more than 250 patients so far with the Linx Reflux Management System magnetic ring since July 2015 in Bern (figures until October 2021). Dr. Jörg Zehetner has worked on more than 5 important studies with the LINX system since 2012, or published as principal investigator of the studies.
Dr. Zehetner also uses the RefluxStop system, which has been known since 2018. Here, on the one hand, the lower sphincter of the oesophagus is held in the correct position in the abdominal cavity by sutures to the gastric fundus, and on the other hand, the fundus is stabilised by a silicone ball (weighing only 9g, 1cm radius). Here, Dr Zehetner includes all patients in a Feasibility&Safety study to collect data on outcomes anonymously and compare them later.
As Dr. Zehetner is currently the only surgeon in Europe who not only masters all 5 reflux operations, but also teaches them to other surgeons, a correct individual therapy for his reflux patients is ensured through a great deal of experience.
Dr Zehetner teaches both modern systems (Linx since 2015, RefluxStop since 2021) in virtual workshops online and on site in Bern at the Beau-Site Clinic.
“From my mentors I have learned “you should have everything in your toolbox”, which means that if you not only know about all the techniques of reflux surgery, but are also an instructor and expert in all techniques, the patient can benefit extremely from my experience” Dr. Jörg Zehetner, Professor
So far, interested surgeons from all over Switzerland, Germany, Austria, Italy, England, Saudi Arabia, Qatar, Dubai, Abu Dhabi, Kuwait, France, Israel and the USA have come to Dr Zehetner’s workshops in Bern.
The LINX workshops were organised with Johnson&Johnson EMEA (Europe, Middle East, Africa), then as online workshops during the Corona situation.
As a preceptor (on-site trainer), Dr Zehetner has been to Switzerland, Austria, Germany and Saudi Arabia several times. Further stays for external workshops are planned in England, France, Dubai and Qatar (December 2021).
Keyword OESOPHAGUS CANCER
In the surgical treatment of oesophageal cancer, too, the minimally invasive technique is not only possible but clearly the better option. As the only attending physician, I use a gentle surgical technique that I learned during more than 200 oesophageal operations in Los Angeles in the USA: Here, the abdomen is operated on “laparoscopically” using the keyhole technique, and if necessary, the dissection in the thorax is performed “thoracoscopically”, and the connection (anastomosis) from the oesophagus to the stomach elevator (as an oesophageal replacement) is always performed on the neck. This is a safe method that can reduce major or life-threatening complications.
I also use a laser-assisted tissue analysis (Pinpoint, Novadaq/Striker) to check the blood flow to the gastric sleeve. In the USA, I was the first surgeon in the world to publish the largest study on this topic in the most prestigious surgical journal (Annals of Surgery, 2015).
“I would be happy to see you in our clinic for an initial discussion of your symptoms and discussion of your previous therapy” Dr. Jörg Zehetner, Professor
Chronic reflux & discomfort
There is a new minimally invasive treatment
The word reflux (Latin for backflow) describes when gastric juice flows back into the oesophagus, causing symptoms such as heartburn (burning in the stomach), acid regurgitation or difficulty swallowing.
At the end of the oesophagus is the lower oesophageal muscle which, if weak, cannot prevent the backflow of acidic gastric juice. The mucous membrane of the oesophagus is not as robust as the stomach, and can not only be irritated by gastric juice (heartburn), but also damaged. There may be infection and scar tissue, but in chronic reflux there may also be cell changes, Barrett’s oesophagus as well as oesophageal cancer. If inflammatory changes are found in a gastroscopy, the risk of developing oesophageal cancer is 44 times higher!
Gastro-oesophageal reflux disease (also called GERD or GORD), is one of the most common diagnoses in Switzerland, with an estimated 20-30% of the western world suffering from acid reflux or heartburn at least once a week.Patients with frequent symptoms have a significant reduction in their quality of life and can be severely restricted in their occupation as well as everyday activities as a result. Translated with www.DeepL.com/Translator (free version)
In addition to the typical symptoms such as heartburn, belching and difficulty swallowing, there are also non-typical symptoms that can, however, also be caused by reflux. These include chronic cough, tooth enamel erosion, chronic sinusitis, lung disease, asthma, vocal cord changes and the feeling of having a lump in the throat. Often a hiatal hernia (where the oesophagus comes from the chest into the abdomen) aggravates the symptoms.
Treatment options
Many patients with minimal symptoms initially take stomach acid blockers (PPI= proton pump inhibitors) to treat the symptoms. However, only the acid in the stomach is partially neutralised, the reflux of gastric juice (including bile) remains. This treats the symptoms but not the cause of the reflux.
Furthermore, the long-term use of PPIs is increasingly viewed critically, as there are indications of a connection with bone fractures (caused by osteoporosis), diarrhoea (caused by Clostridium difficile) and oesophageal cancer.
Especially in patients where drug therapy is insufficient to alleviate the symptoms, a consultation with a surgeon should take place. An individual consultation after diagnostic clarification then results in one or more surgical treatment options.
All surgical procedures can be performed minimally invasively (keyhole surgery). Nissen or Toupet fundoplication are more complex operations where a gastric sleeve is placed around the end of the oesophagus to prevent reflux. The sleeve can be applied either completely (Nissen fundoplication) or partially (Toupet fundoplication).
New is the Linx Reflux Management System, which was developed before 2007. Since 2012, it has also been used outside of studies in selected reflux centres in Europe and the USA, i.e. for almost 10 years.
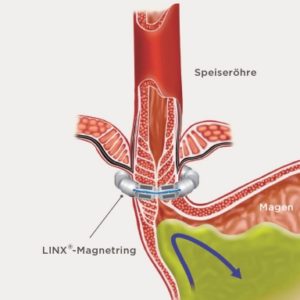
Fig. 1 The LINX® system helps the oesophagus resist opening, preventing or reducing reflux.
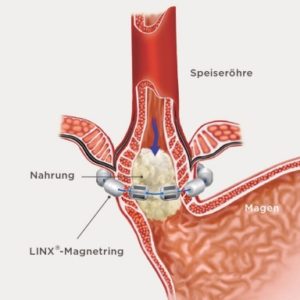
Fig. 2 The LINX® system stretches to allow normal swallowing.
Since 1 July 2015, Dr Jörg Zehetner has been able to offer the Linx magnetic ring (LINX Reflux Management System) at the Beau-Site Clinic, the only centre in the canton of Bern.
This small implant is placed around the lower oesophageal muscle via laparoscopy. It is a small, flexible band of linked titanium beads with magnetic cores. The force exerted during swallowing briefly separates the balls. When closed, no reflux is possible, but at higher pressure (regurgitation of air or vomiting) the ring opens. At the same time, any diaphragmatic hernia is also operated on during this operation. Depending on the size of the diaphragmatic hernia, 2-3 sutures are placed here, or a special mesh is also used. These meshes are either rapidly absorbable (dissolve) within 6-12 weeks, or slowly absorbable within 10-18 months. The surgeon makes the selection during the operation based on the tissue condition. This is where the surgeon’s experience plays a big role.
Dr Jörg Zehetner is one of the few surgeons in Switzerland who has experience with all absorbable meshes and has also conducted studies.
What examinations are needed before an operation?
Diagnosis of reflux disease requires a gastroscopy (gastroscopy) and a swallowing X-ray, as well as pH monitoring (acid measurement): This involves measuring the acid in the oesophagus over 24 or 48 hours (outpatient examination). A so-called DeMeester score takes several factors into account and describes the severity of the reflux (normal value is below 14.7).
If the examinations have not yet been carried out elsewhere, we can arrange for them to be carried out in our “Reflux Centre”. The Reflux Centre is a cooperation between Swiss1Chirurgie AG and the gastroenterological partner practice of GGP Bern AG. Both clinics are part of the Helvetius Holding AG network.
The collaboration between the surgeons and gastroenterologists creates an exceptionally high level of expertise from which reflux patients can benefit. We are the only centre in addition to the University Hospital to have all the possibilities for functional assessment of the oesophagus, including manometry, pH-metry and also the Endoflip examination, which we can perform exclusively at the Beau-Site Clinic. More information on this can also be found at www.ggp.center.
Who is the Linx Reflux System suitable for?
If the oesophagus functions normally on swallowing x-ray or manometry, the Linx system is a good option; if oesophageal function is reduced, a laparoscopic partial cuff (fundoplication) is recommended. For very large diaphragmatic hernias, repair of the diaphragmatic hernia with mesh plus laparoscopic Nissen fundoplication or Toupet fundoplication is usually the standard operation.
So if you are not completely free of symptoms despite medication or have concerns about taking PPI for a long time, it is definitely worth seeing the surgeon directly. A visit to a specialist is necessary in order to receive the optimal individual treatment with different therapy options.
Every second person knows the burning pain behind the breastbone. Heartburn! The cause is food pulp mixed with stomach acid and liquid that flows back into the oesophagus through the unclosed stomach sphincter. This is called reflux disease. The LINX™ reflux management system can remedy this and eliminate the effects of reflux disease by means of minimally invasive surgery. We can tell you whether LINX™ can help you after an individual examination.
Chronic heartburn is not only unpleasant, it also robs you of any quality of life. At night you can’t sleep because of the burning in your chest and during the day you have to burp constantly. This is where the LINX™ reflux management system can help. The LINX™ ring is placed minimally invasively around the sphincter of the oesophagus, closing the stomach. The stomach acid remains in the stomach and your complaints disappear permanently.
Acid regurgitation during the day is only one symptom of reflux disease. At night, the burning in your chest robs you of sleep and you no longer enjoy eating. Constant throat clearing and a dry mouth are other symptoms that your stomach sphincter is not closing the stomach properly. Stomach acid rises and the oesophagus becomes inflamed – reflux oesophagitis, as the experts say. We can help you. After a personal examination, we can tell you whether you are suitable for the LINX™ reflux management system or whether another therapy is advisable.
LINX™ & Themes
In reflux disease, there is a weakness of the oesophageal sphincter. This causes acid and bile to flow from the stomach into the oesophagus. If left untreated, reflux disease can have serious consequences later on: Heartburn, nausea and occasionally vomiting are the initial signs of the disease. The long-term reflux of acidic gastric juice can lead to an infection of the larynx and the upper airways, possibly chronic bronchitis with asthma-like symptoms and even the development of mucosal ulcers. Now there is a gentle, fast-acting treatment method for the patient, the LINX™ reflux management system.
Esophagitis – inflammation of the oesophagus
While acid in the stomach is normal and usually tolerated by the stomach, the oesophagus is not suitable for prolonged exposure to acid. The “regurgitation” of acid, also called heartburn, is called reflux.
The oesophagus can become irritated with increased reflux and is referred to as mild, moderate and severe infection (oesophagitis).
The diagnosis is made with an endoscopy (oesophagoscopy and gastroscopy).
therapy:
The initial therapy is to take PPI (acid blockers) so that the infection heals within 2-4 weeks. A visit to a surgeon is also necessary to discuss whether reflux surgery is an option.
Barrett’s oesophagus
Any change visible in the endoscopy is biopsied (a minimally small sample is taken). If there are visible changes at the lower end of the oesophagus, the tissue may be altered in the sense of a precancerous condition.
A distinction is made here between low-grade and high-grade dysplasia (change).
Depending on the findings, these changes may need to be removed or followed up with 6-12 month check-ups.
Barrett’s oesophagus is when there is a visible cell change at the end of the oesophagus. This is caused by chronic reflux and can also be present in patients who are completely symptom-free.
Therapy: If necessary, this altered mucosa can be removed either endoscopically or endoscopically with radiofrequency technology (with halo balloon). Here, our specialists in the partner clinic www.ggp.center are at your disposal, especially PD Dr. Merki and Dr. Linas are familiar with this method.
Subsequently, either a long-term medication therapy with PPI or a surgical rehabilitation of the reflux problem is necessary.
Diaphragmatic hernias
A distinction is made between hiatal hernias and paraesophageal hernias.
Basically, these hernias (ruptures) are caused by a weakness of the diaphragm, whereby part of the stomach slips upwards into the chest.
This makes it easier for the lower closure of the oesophagus to give way, often resulting in chronic reflux.
Some patients may experience acute incarceration and life-threatening symptoms. Some patients lose blood steadily due to infection in this area, and the diagnosis is only made during an anaemia work-up.
therapy:
Small hiatal hernias up to 3cm in size without symptoms do not require surgical treatment. However, in patients with reflux or larger hernias, surgery is necessary, which can be performed laparoscopically (laparoscopy). By means of 4-5 small incisions in the abdomen, this operation can usually be performed laparoscopically in 1-1.5 h, the hospital stay is usually 1-3 days. After the operation, a slow build-up of food is necessary, with first liquid, then mushy food for about 2 weeks.
Achalasia
This disease is a lack of peristalsis of the oesophagus with usually high pressure in the lower oesophageal obstruction. The oesophagus cannot cause coordinated forward movement of the food. This causes food to linger in the oesophagus, be regurgitated or vomited up. Other complaints are pain in the chest or upper abdomen, or a feeling of tightness in the throat. The diagnosis is made with a contrast medium X-ray swallow or a pressure measurement of the oesophagus (manometry).
therapy:
Unfortunately, there is no useful drug therapy available. There are endoscopic procedures (balloon dilatation) as well as surgical procedures (laparoscopic myotomy).
In the minimally invasive method with laparoscopy, 4-5 small incisions are made in the abdomen and then the lower oesophageal muscle is split in a 1-hour operation. This allows the food to pass from the oesophagus into the stomach again without resistance. As a rule, the inpatient stay lasts no more than 1-3 days.
Benign diseases of the oesophagus
Here we distinguish between the above-mentioned diseases and changes in reflux, as well as other rare diseases such as lipomas or leiomyomas, and diverticula of the oesophagus.
Diverticula (bulges) of the oesophagus do not necessarily cause problems. However, they are usually discovered by the patient experiencing difficulty swallowing, frequent belching or heartburn.
These bulges can occur in the throat or at the end of the oesophagus. Very rarely, they are also found in the middle of the oesophagus, then usually caused by diseases or changes in the lymph nodes located there.
Protrusions in the neck are called Zenker diverticula. These are caused by weakness in the oesophageal muscles.
Treatment can be either endoscopic or surgical.
Malignant diseases of the oesophagus
The 2 most common types of oesophageal cancer are squamous cell carcinoma and adenocarcinoma.
While squamous cell CA is caused by smoking and alcohol, reflux plays the main role in adeno-CA. Patients with reflux changes in the oesophagus have a 44 times higher risk of developing cancer than the normal population.
The initial symptoms are often belching and heartburn, but more often difficulty swallowing. The diagnosis is made with an endoscopy. An ultrasound examination of the oesophagus and CT (computer tomography) of the chest and abdomen are also necessary in order to make an exact therapy plan and prognosis.
If the cancer is only superficial in the uppermost layers of the mucosa, it can also be removed endoscopically.
For tumours in deeper layers, the decisive factor is whether lymph nodes are also affected. Chemotherapy and radiation with subsequent resection of the oesophagus is then recommended. Today, the removal of the oesophagus can also be carried out minimally invasively in selected cases. The oesophagus is then replaced by a tubular stomach elevator.
The operation takes between 3 and 6 hours and the hospital stay is usually between 5 and 10 days.
In the case of tumours affecting other organs, chemotherapy is useful; surgical methods are only used to alleviate the symptoms. These include the placement of feeding tubes in the stomach or small intestine, as well as the insertion of a stent in case of swallowing difficulties or the dilatation of a constriction by means of an endoscopic balloon.
Here, too, it is crucial to talk to the surgeon quickly and at an early stage in order to receive optimal care and individual therapy.
Stomach inflammations
Acidity in the stomach can also cause problems in the stomach.
Chronic use of painkillers (NSAIDS such as Voltaren, Toradol or aspirin) can lead to gastritis. In severe cases, gastritis can result in an ulcer with possible perforation.
The diagnosis is made endoscopically. If the stomach is colonised with the Helicobacter pylori germ, eradication therapy should be carried out (2 different antibiotics and a PPI acid blocker).
However, gastritis can also be stress-related. Other reasons can be a gastric emptying disorder or tumours in the pancreas. Other risk factors may include smoking and excessive alcohol consumption.
Benign diseases of the stomach
Ulcers do not have to be malignant. They can be caused by medication, stress or alcohol and usually heal with therapy with PPI acid blockers.
Polyps (small, stalk-like growths) can be benign as a result of taking acid blockers for many years.
Lipomas or leiomyomas are rarely found in the stomach wall and can often be removed laparoscopically.
Malignant diseases of the stomach
Stomach cancer is often detected late, often the visit to the doctor only takes place when weight loss and loss of appetite occur. The diagnosis is made by endoscopy, but for therapy planning, a CT (computer tomography) of the abdomen and pelvis is also needed.
Endoscopic therapy can rarely be used for early stages. It is usually possible to remove part of the stomach, or even the whole stomach, by means of laparoscopy. The oesophagus or residual stomach is then directly connected to the small intestine.
SIMPLY EXPLAINED
Film reports & lectures on acid reflux, oesophageal cancer, aftercare and other medical topics.