Obesity and sport
Pathological overweight? Obesity? Is sport still possible here? What is it like after obesity surgery?
Ariane and Tanja tell us about their journey from being overweight to surgery, the advantages and disadvantages, the importance of aftercare, and what they do now in terms of sport.
Cooperation with Dr. Ulf Kessler in Lausanne
Visceral surgeon Dr. Ulf Kessler has been at Hirslanden Clinique Cecil as an attending physician for more than a year, and has his practice at CMD Lausanne. With his extensive experience in visceral surgery, he is a competent partner for Swiss1Surgery with Dr. Jörg Zehetner, Professor (USC), in the special field of reflux surgery, as well as surgical intervention with the LINX Reflux Management System.
With the cooperation of Dr. Ulf Kessler and Swiss1Chirurgie, the range of services for the use of the LINX Reflux Management System can now also be offered in Lausanne. In this way, we are extending our radius of action to western Switzerland in the interests of our patients.
In March 2022, the collaboration between Dr. Jörg Zehetner and Dr. Ulf Kessler successfully treated a patient with the LINX Reflux Management System for the first time at the Hirslanden Clinique Cecil in Lausanne. The 45-minute operation was minimally invasive and the patient was discharged from the hospital after two days without any symptoms.
What’s new?
Dr. Zehetner has already performed 350 surgeries with the LINX Reflux Management System in Bern since 2015. This surgery is considered for all patients with typical reflux symptoms, small to moderate diaphragmatic hernia and with normal esophageal function. Now this surgical technique, which has been tried and tested worldwide for ten years, is also available to patients in French-speaking Switzerland.
With Dr. Ulf Kessler, an ideal partner for such interventions was found. Dr. Ulf Kessler was in training for a period of three years to specialize in visceral surgery at the Hirslanden Klinik Beau-Site in Bern, and has already worked with Dr. Jörg Zehetner – as the responsible tutor for Upper GI Surgery and Bariatric Surgery.
During this time, the results of the first 150 operations with the LINX system were also published in Bern. Dr. Kessler’s scientific collaboration was a key factor in the success of the project. In the Hirslanden Center for Digestive Diseases in Lausanne, an ideal partner was found for Western Switzerland, especially since important accompanying specialties such as endoscopy and gastroenterology/hepatology are also on site there.
Interested patients and affected relatives from Western Switzerland can contact Dr. Kessler directly in the future. With his team on site in Lausanne, Dr. Kessler will then perform the assessment and, in collaboration with Swiss1Surgery with Dr. Zehetner, perform any surgical procedures using the LINX Reflux Management System.
Through this collaboration, the good care during the clinic phase and also the follow-up by an experienced specialist can be guaranteed.
The cooperation between Swiss1Surgery and Dr. Ulf Kessler is groundbreaking for this field. This means that the expertise of Dr. Jörg Zehetner, who has the most experience with the LINX system in Switzerland to date, can also be made available to patients in French-speaking Switzerland.
For patients with special questions, the Swiss1Surgery practice in Bern and the GGP Gastroenterology Group Practice with its special functional diagnostics naturally remain a direct and good point of contact.
For further questions we gladly refer to the website www.swiss1chirurgie.ch


World Obesity Day 2022 – All must act
Under the motto “Everybody needs to act”, World Obesity Day on 04 March 2022 will mark the start of a new year in the fight against the global spread of obesity as one of the most threatening diseases of all. In the meantime, more people worldwide suffer from obesity than from hunger. There is more personal and societal suffering and damage associated with the widespread disease of obesity than is assumed. To learn more about World Obesity Day on March 04, 2022, and what we can all do, read Swiss1Chirurgie’s in-depth article.
March 04 is World Obesity Day– Let’s all get active!
The tireless campaign against obesity is a global, but also a personal task
Yes, with “tireless effort” we have probably made a somewhat unusual choice of words, but with all good reasons. Obesity is an exorbitantly increasing disease of civilization everywhere in the world. In the meantime, more people worldwide are affected by overweight and obesity than, on the other hand, people suffer from hunger. And that with all the consequences for individual health, for societies and for the development of humanity in general.
Understanding obesity as the affliction of our time
For World Obesity Day on March 4, 2022, we want to specifically and deliberately draw attention to the global disease of obesity. The effects that obesity has on personal life and virtually all areas of life and society are now fatal, but are communicated publicly far too rarely and with far too little energy.
Obesity literally makes life difficult, imposes extensive restrictions on personal life, inflicts economic damage, and burdens both health care systems and very personal lives. In particular, the frequency and intensity of concomitant and secondary diseases associated with overweight and obesity are becoming increasingly apparent. From cardiovascular disease to psychological problems to premature death, there is a breadth of manifestations inextricably linked to obesity.
Only then, when we understand obesity as the suffering of our time, will we also be able to understand the worldwide fight against obesity as a task for humanity. Well-intentioned advice, declarations of intent and the often reluctant renunciation of too much are not enough. It’s time to take action.
All must act
“Jeder muss handeln” – Das ist das Motto des World Obesity Day 2022. Everyone must act, however, also means that everyone must finally take action now. It is not only people suffering from obesity who are addressed. Also addressed are those who are indirectly or directly involved in the further spread of the widespread disease of obesity. Here we address the food industry, retailers, advertisers and consumers as well as politicians, interest groups and society as a whole.
Only when we understand that obesity is a key health and societal problem will we be able to achieve appropriate diversity of action and activity. The time for explanations and goodwill is over. If obesity is not ultimately to become the scourge of humanity, we must all take action now, and all together.
What to do
In a whole series of articles, Swiss1Chirurgie and the Center for Bariatric Surgery, together with its partners, have so far devoted themselves to the topic of obesity, the risks and the treatment options. In doing so, we have always focused on prevention. What we do know is that words alone are not enough.
Now, finally, it comes down to everyone’s actions. Those affected, doctors, scientists, food producers, politicians, families, friends and the whole of society are called upon if the fight against obesity with all its consequences is to succeed.
This requires above all real activity, not only good words and not only on March 04. But let’s all make March 04, 2022 the start of a global movement against obesity. All of you, mark this day down as the start day to a better and healthier life.
Let us support those affected by listening carefully to them, perceiving and understanding them in their problem situation. Let’s stop stigmatizing fat people and portraying them as lazy and to blame. Let’s start by providing these people in particular with active and useful aids for everyday life. In case of emergency, this also includes medical and psychological accompaniment, but above all a lift to an active and healthier life.
Living better doesn’t have to mean simply doing without. With numerous opportunities and activities, individuals, associations, companies and friends can help to create new perspectives for the overweight people. In doing so, we are not only showing that we understand obesity as a disease, but that we are all willing to join forces in the fight against obesity.
We as Swiss1Chirurgie together with the Center for Bariatric Surgery see ourselves as partners of the overweight and at the same time as supporters of all those who support us in the fight against global obesity. To this end, we inform and act not only in our clinics, but also in a series of lectures, in our publications and, above all, in our direct work with people.
World Obesity Day on March 04, 2022 can be the start of a new understanding of obesity and action against it. But only if we actually all act. Because every life is a life worth living.
Thun is another Swiss1Surgery site
With the clinic of Dr. Markus Naef in Thun, Swiss1Chirurgie puts its range of services on an even broader footing and ensures professional care for patients in this region as well. With Dr. Naef, we were able to gain an integral partner who has been working successfully in bariatric surgery in the Thun region since 1998 and is extremely familiar with all modern techniques in obesity surgery. Read the article to find out what this means for patients in Thun and the surrounding area and how we are thus further implementing our 360° claim.
New partner practice in Thun cooperates with Swiss1Chirurgie
As is well known, the squaring of the circle consists of exactly four quarters. And a circle has an angular measure of 360°. With the integration of the clinic Dr. Naef in Thun, we are integrating a fourth partner into Swiss1Chirurgie and at the same time underlining our 360° approach in the interest of our patients.
We are successfully expanding patient care
In addition to our previous Swiss1Chirurgie practices in Solothurn, Bern and Naters in the Valais, we have now been able to gain Dr. Markus Naef with his clinic for general surgery/visceral surgery as an integral part of Swiss1Chirurgie. With its focus on bariatric surgery, Dr. Naef’s clinic completes our service portfolio at another location. The beneficiaries of this cooperation, which is very gratifying for us, are above all the patients, who can now enjoy even better care, especially in the field of obesity surgery. This is a step that can help to meet the constantly growing demand for obesity surgery, including detailed consultation, pre-surgery care and aftercare, especially in such complex and consultation-intensive fields as obesity surgery.
Who is Dr. Markus Naef
Dr. Markus Naef is a true Thun native. His connection to his home region provides him with an excellent network in the Oberland and has long made him a sought-after specialist in visceral surgery and obesity surgery. Dr. Naef opened his clinic in Thun in 1998. Since then, he has enjoyed a high level of acceptance among patients from Thun and the surrounding area. As past president of the SMOB (Swiss Society for the Study of Morbid Obesity and Metabolic Disorders), Dr. Naef has not only established an exceptionally good reputation among his peers, but has also played a decisive role in shaping treatment guidelines.
His wide range of experience includes techniques commonly used in bariatric surgery such as gastric bypass, tubular stomach, gastric banding, vertical gastroplasty, revision surgery and others. Thus, the clinic of Dr. Naef in Thun fits perfectly into the range of services of Swiss1Chirurgie and can be an excellent extension of the services of Swiss1Chirurgie in Thun at its location.
With the integration of a fourth site into Swiss1Chirurgie, we are rounding out our circle. With the now broad and specialized range of services in Thun, we continue to pursue our 360° claim,with which we want to reach, advise, treat and care for our patients preferably where they live. For patients in the Thun region, this means that they can now also take advantage of the excellent services of Swiss1Chirurgie in association with other specialist centers in Thun with the clinic of Dr. Naef.

The clinic is located in the Denner building opposite Thun train station (less than 5 minutes walk) at Frutigenstrasse 16, 3600 Thun, on the 2nd floor (elevator, wheelchair accessible).
Swiss1Chirurgie wishes everyone a Happy New Year
We combine these wishes with a clear request: to rethink our own health and lifestyle. Instead of good resolutions, which usually only survive New Year’s Day, you should perhaps start with concrete steps. How about a visit to the family doctor or specialist? A simple thing with only a few restrictions but great effects. Read the New Year’s greetings from Swiss1Chirurgie here.
A healthy new year often begins with rethinking
First and foremost, we would like to thank all our patients, partners, referring doctors and our many interested parties for their interest in our work. We combine this thanks with best wishes for a peaceful, happy and above all healthy year 2022.
A new year often begins with new good intentions. Quitting smoking, exercising more and losing weight are just a few of the good intentions that many people make. However, we also know from experience that such good resolutions often have a half-life of only a few hours to a few days. Far too quickly we fall back into old habits. It’ll be fine.
It is rewarding to perhaps start the new year with a rethink on many health issues. This can then also be the first best step towards a healthier life. From a medical perspective, at Swiss1Chirurgie we deal with conditions such as obesity, reflux, oesophageal cancer, bariatric surgery, hernias and non-alcoholic fatty liver.
In most cases, we already see in the anamnesis that many clinical pictures and symptoms are very closely related to the lifestyle we have chosen for ourselves. Accordingly, it is also up to each person to tackle certain possible changes in life. More exercise in everyday life and sport in leisure time, healthier eating and drinking, abstaining from nicotine and alcohol are always the first good steps towards a healthier and often longer life.
Many diseases we only notice when it is apparently already too late. This also includes liver diseases, which in many cases are due to an unhealthy diet that is too fatty and too sugary. We do not feel the effects on the liver itself at first. But the interactions on many other organs. Liver health is one of the most important issues in internal medicine. So what’s stopping us from taking more care of our health in the new year? The beginning can be liver fasting, which we have already presented, for example, in the series of lectures Helvetius.events at the specialist conferences of Helvetius Holding AG in 2021. Here you can re-live the lecture.
By rethinking health and taking the first concrete steps, everyone is making a simple but very effective contribution to making 2022 a healthier year. The beneficiaries are not only yourself, but also your family, friends and colleagues.
With this in mind, we wish you all a good year 2022, which should in the best case start with a rethink about your own health.
New Swiss1Chirurgie location in Valais
New on 1.1.2022 – Bahnhofstrasse 20/22, 3904 Naters
Improved surgical care in Valais will be available from 1.1.2022 with the new location of Swiss1Chirurgie in Valais in Naters. With its specialised services, Swiss1Chirurgie is thus expanding its range of services.. Good news for patients as well as for referring physicians. The new location in Naters concentrates primarily on preventive care, diagnostics and aftercare, while surgical procedures are performed in Bern. Read more about the new Swiss1Chirurgie location in Naters here.
Swiss1Chirurgie also treats patients in Valais
On 1.1.2022, Swiss1Chirurgie will open a new clinic at a new address in the Valais, namely in Naters. In addition to the locations in Solothurn and Bern, this will also strengthen patient care in the canton of Valais.
For many years now, Swiss1Chirurgie has established itself in Switzerland as a medical centre with a wide range of specialised services and inspires referring physicians and patients with its extremely professional team and range of services. In order to be able to further expand this offer in the Valais, it has now been agreed to locate the centre in Naters. The main focus here will be on thorough diagnosis, prevention and follow-up care, with the necessary procedures being carried out in the tried and tested manner in Bern.
What Swiss1Chirurgie now also does in Valais
Swiss1Chirurgie is known for its broad yet specialised range of specialist services. In general surgery, the focus here is on inguinal hernias, abdominal wall hernias, gallstones and diverticulitis. Equally extensive are the services relating to tumours of the small and large intestine, in thyroid surgery and in proctology. The services in general surgery are supplemented by so-called minor surgery, for example in the treatment of skin lesions.
Typical services provided by Swiss1Chirurgie in the field of visceral surgery are no less interesting. Reflux operations, diaphragmatic hernias, oesophageal and gastric tumours can then also be treated in Bern after diagnosis in Naters. Liver surgery and colon surgery including deep rectal tumours expand the range of services, as does the broad field of obesity surgery.
This means that Swiss1Chirurgie has long since established itself in specialist circles as a reliable and professional partner and now also provides comprehensive care and advice for patients in Naters for the entire Valais. Of course, we are also fully available to advise referring doctors.
Swiss1Chirurgie app summarises all services and offers a plus in information
We have compiled all the services of Swiss1Chirurgie, lots of comprehensive information and, of course, all the contact options in a convenient app. Here there is even the possibility of individualised information for both patients and referring physicians. In this way, we are responding to people’s desire to also have expert knowledge available everywhere and are giving referring physicians in Valais the opportunity to provide the best treatment for their patients in each case.
For Valais, the Swiss1Chirurgie site in Naters means an even broader range of specialised services. As already noted, in Naters we focus in particular on the prevention, diagnosis and follow-up of diseases in the respective areas and are happy to refer to our location in Bern for surgical interventions.
For questions and further information, please use our Swiss1Chirurgie app or contact us directly.
Reflux and oesophageal cancer – An inside view
Vom 21. bis 27. November 2021 läuft die GERD Awareness Week. GERD steht für Gastroesophageal Reflux Disease, also kurz gesagt die Refluxkrankheit. Betroffen davon sind etwa 20 Prozent der Bevölkerung. Das individuelle Erscheinungsbild und Ausmass kann dabei sehr unterschiedlich ausgeprägt sein. Wir wollen anlässlich der GERD Awareness Week den Blick auf die Refluxkrankheit, mögliche Folgeerkrankungen und eine zielgerichtete Diagnose und Behandlung richten. Dabei ist uns die ganz persönliche Sicht Betroffener ebenso wichtig wie die Möglichkeiten der chirurgischen Intervention und die Chancen der Vorsorge und gezielter Nachsorge.
Saures Aufstossen ist mehr, als nur unangenehm
Im Rahmen der GERD Awareness Week setzt die Swiss1Chirurgie noch einmal verstärkt auf die Aufklärung zu Refluxerkrankungen, die sich oftmals durch chronisches saures Aufstossen ankündigen oder bereits vorliegen. Von der ersten individuellen Wahrnehmung über eine fachmedizinische Diagnostik bis hin zur chirurgischen Intervention reicht die Spannbreite der Wahrnehmung von Refluxerkrankungen, die zumindest in bestimmten Bevölkerungsgruppen weiter auf dem Vormarsch sind. Mehr zum Thema lesen Sie im Beitrag.
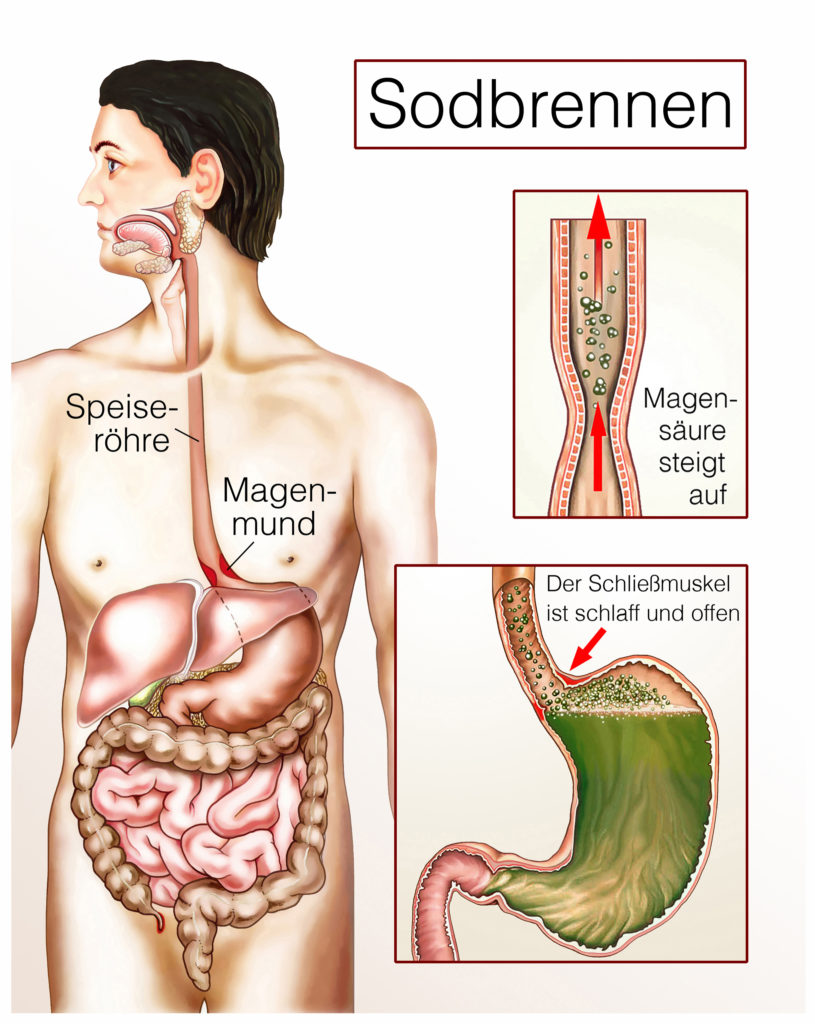
Saures Aufstossen, die persönliche Sicht
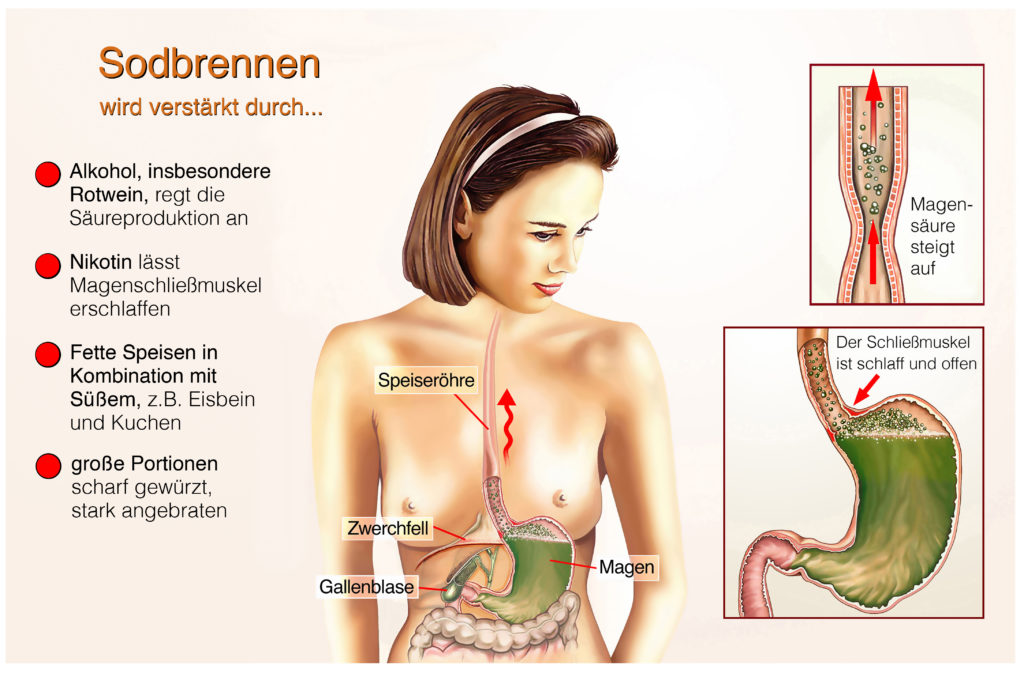
Upps, da ist es wieder. Dieses unangenehme Aufstossen von saurem Magensaft mit diesem bekannt widerlichen Gefühl. Magenflüssigkeit und im Einzelfall auch Nahrungsbestandteile steigen vom Magen in die Speiseröhre auf und sorgen neben dem bitteren Beigeschmack für ein Gefühl des Unwohlseins. Besonders nach üppigem, fettreichen oder scharfen Essen klagen viele über das sogenannte Sodbrennen, machen sich aber wenig Gedanken, darüber, wo die Ursachen zu suchen sind und welche Folgeerscheinungen möglich sind. Übrigens tragen auch Alkoholkonsum, deutliches Übergewicht und das Rauchen zur Ausbildung und Verstärkung von Refluxerkrankungen bei. Richtig lästig wird es, wenn dieses saure Aufstossen immer häufiger und wiederkehrend auftritt. Dann reden wir bereits vom chronischen Aufstossen, das durchaus Krankheitswert haben kann. In der Endkonsequenz wird es wichtig sein, jetzt einen versierten Mediziner zu finden, der sich mit der Diagnose, Behandlung und Nachsorge der Refluxkrankheit tatsächlich gut auskennt. Der erste Weg ist dann meist der zum Hausarzt, der dann als Zuweiser die passenden Fachmediziner finden sollte. Wichtig ist in jedem Fall, chronisches saures Aufstossen nicht auf die leichte Schulter zu nehmen, sondern frühzeitig die fachmedizinische Sicht einzuholen. Denn aus anfangs gelegentlichem Aufstossen kann schnell mehr werden, mit entsprechend schwerwiegenden Folgen.
Wenn aus chronischem Aufstossen Krebs wird, die medizinische Sicht
Der Weg vom chronischen Aufstossen bis zum Speiseröhrenkrebs ist in vielen Fällen kürzer, als gemeinhin angenommen. Durch den wiederholt in der Speiseröhre aufsteigenden Magensaft wird die empfindliche Schleimhaut der Speiseröhre angegriffen und ernsthaft geschädigt. Im weiteren Verlauf entwickeln sich Zellwachstumsstörungen, die im Ernstfall zu unkontrolliertem Zellwachstum und damit zu Speiseröhrenkrebs führen können.
In einem frühen Stadium spürt der Patient davon kaum etwas, sodass nur eine zeitige medizinische Diagnose und Intervention Aufschluss bieten und eine adäquate Behandlung sicherstellen kann. Ist die Speiseröhre bereits stark geschädigt und ein deutliches Krebswachstum vorhanden, äußert sich das bei den Patienten durch deutliche Schluckbeschwerden und gegebenenfalls auch mit einem Druckgefühl im Brustbereich, dass vom Patienten selbst jedoch kaum klar lokalisiert werden kann. Hier ist dann dringlichst eine fachmedizinische Diagnose erforderlich, um eventuell noch rechtzeitig eingreifen zu können. Ein Hinwarten verbessert die Situation nicht, sondern führt eher zu einer verschlimmerten Gesamtsituation.
Daher ist es in jedem Fall von gehäuftem sauren Aufstossen ratsam, baldigst einen Fachmediziner aufzusuchen, um im diagnostischen Prozess die konkrete Lage und eine eventuelle Gefährdungssituation professionell abschätzen zu können. Mit handelsüblichen Präparaten gegen Sodbrennen lässt sich der Prozess zwar mildern, aber nicht effektiv aufhalten oder beenden.
Chirurgische Intervention, der notwendige Eingriff
Ist ein chirurgischer Eingriff bei einer Refluxerkrankung erforderlich, dann greifen die Experten der Swiss1Chirurgie bevorzugt auf minimalinvasive Operationsmethoden zurück. Dabei wird nicht am Symptom, sondern an der Ursache angesetzt. Die Ursache für das chronische saure Aufstossen ist häufig am Übergang zwischen Speiseröhre und Magen und oftmals auch im Durchgangsbereich am Zwerchfell zu suchen. Das, nennen wir es Ventil am Mageneingang schliesst nicht mehr richtig oder ist in seiner Funktion anderweitig beeinträchtigt, so dass immer wieder saurer Magensaft nach oben steigen kann. Nicht selten ist auch die Pumpfunktion der Speiseröhre gestört, was sich in einem Funktionstest ermitteln lässt.
In der Swiss1Chirurgie wird nach Möglichkeit ein System eingesetzt, bei dem ein elastischer Magnetring um das Speiseröhrenventil gelegt wird. Dieser Magnetring verschliesst den Übergang von Speiseröhre zum Magen, erlaubt aber das normale Aufnehmen von Nahrung, sofern der Druck in der Speiseröhre normal ist. Auch ein leichtes Aufstossen von Luft bleibt möglich.
Über dieses Verfahren und andere Möglichkeiten der Behandlung von Refluxerkrankungen können Sie sich umfassend und komfortabel auf unserer Webseite informieren.
Gefährdete Gruppen und Tendenz
Von Refluxerkrankungen sind vor allem Menschen betroffen, die Schwächungen am Übergang von der Speiseröhre zum Magen aufweisen. Eine grosse Gruppe der Patienten rekrutiert sich aus der Gruppe der übergewichtigen Menschen. Wenngleich das nicht das alleinige Risiko abbildet, ist Übergewicht doch ein entscheidender Faktor bei Refluxerkrankungen. Auch übermässig fettes und scharfes Essen provoziert Refluxstörungen ebenso wie der übermässige Alkoholkonsum oder das Rauchen.
Tendenziell kann davon ausgegangen werden, dass Refluxerkrankungen weiter zunehmen werden. Ursache dafür sind das Ernährungsverhalten der Menschen und der übermässige Gebrauch von Genussmitteln. Eine insgesamt gesunde Lebensweise kann auch Refluxerkrankungen vorbeugen, wenngleich auch anscheinend gesund lebende Menschen davon betroffen sein können.
Was zu tun bleibt
Wer bereits über Refluxbeschwerden klagt, sollte insbesondere sein Essverhalten überprüfen. Fettiges Essen, grosse Portionen, saures und scharfes Essen sollten ebenso vermieden werden wie ein Zuviel an Kaffee, Schokolade, Alkohol und Nikotin. Eine Gewichtsreduktion ist in vielen Fällen ratsam.
Sollten sich auch dann keine kurzfristigen Verbesserungen einstellen, ist der Gang zum Hausarzt oder direkt zum Experten für Refluxerkrankungen unerlässlich. Nur dort kann die Situation klar und eindeutig abgebildet werden, was schlussendlich der sicherste Weg zu einer zutreffenden Diagnose und einer nachfolgenden Behandlung ist.
Auch zu den Möglichkeiten der Beeinflussung von Refluxerkrankungen finden Sie auf unserer Webseite umfangreiches Material.
Für Fachkollegen empfehlen wir die Teilnahme am Zuweiserevent am 25. November 2021 im Rahmen der GERD Awareness Week 2021.
Martin Andermatt with his experiences on liver fasting
When Martin Andermatt talks about his experiences with liver fasting, the football legend and FC Schaffhausen coach is mainly talking about experiences with himself. The core of his presentations is that something only changes if you change yourself. This is just as true in active sports as it is in maintaining the health of one’s own body. The well-known Swiss also shares this experience at the 4th Helvetius Holding AG symposium at the Talent Campus Bodensee in Kreuzlingen. Read the report here and find out where you can watch the live stream.
A field report on liver fasting with HEPAFAST® by Martin Andermatt
Dr. med. Jörg Zehetner, Professor (USC), and Dr. med. Hardy Walle spoke on the topic of liver health and fatty liver at the 4th specialist conference of Helvetius Holding AG at the Talent Campus Bodensee Kreuzlingen. The highlight of the evening was undoubtedly the lecture by Dr. Hardy Walle, MD, who not only used the latest scientific approaches to shed light on non-alcoholic fatty liver from a somewhat different perspective, but was also able to present an effective concept for liver fasting in the form of HEPAFAST®.
In the following, football legend Martin Andermatt reported on his own experiences of liver fasting with HEPAFAST®. As a successful professional footballer and now coach of FC Schaffhausen, Martin Andermatt knows very well how important stable health is and what effects a healthy liver has on the entire organism.
As a football coach, Martin Andermatt likes to talk about his own practical experiences. With his own experience, Martin Andermatt was the first Swiss coach of a German Bundesliga team and also knows the German league business from the perspective of a supervisory board member at the Hannover 96 club.
In line with his own sporting career, also as an active player, Martin Andermatt has always been interested in how a good, balanced and healthy diet can be designed. As he got older, the question of how to continue in life after active football also came into focus. The main interest was in the physical and psychological effects of no longer exercising so intensively and practically losing a previously accustomed amount of exercise.
As a coach, Martin Andermatt also sees his responsibility in conveying information to adolescent and also adult players that is also correct and underpinned. Conjecture, hearsay and supposed knowledge are not really strong arguments. That is why Martin Andermatt knows very well that only one’s own experience is a good basis for passing on knowledge. He also sees this fundamental approach as important when he gives his very own experience report on liver fasting with HEPAFAST® at the 4th Helvetius Holding AG symposium.
Even though Martin Andermatt, as a non-medical doctor, does not know the formulas for liver health, he was able to follow every step in the lectures by Dr. med. Jörg Zehetner, Professor(USC), and Dr. med. Hardy Walle, founder of BODYMED and co-developer of liver fasting with HEPAFAST®. Especially from his own experience.
Personal experience is what really counts
Martin Andermatt also knows from his experience with liver fasting that this is not simply a matter of doing things quickly for a short time. It is always important to look at the development. Martin Andermatt sees this in his sporting commitment as well as in his personal attitude to health. However, even here beautiful and melodious words are always worth less than one’s own experience. And this is exactly how Martin Andermatt reports on his own experience with liver fasting with HEPAFAST®.
His first observation is about the dream world. For example, he reports that he dreamed much more intensely than usual during the periods of liver fasting. In addition, he felt extremely vital and efficient in every phase of the liver fast.
With now already 60 years of life experience, Martin Andermatt still feels very well today and knows that he has already tried a lot of things regarding health maintenance. Be it juice cures or various diet programmes. Martin Andermatt knows what he is talking about when he passes on information to his athletes.
Especially with regard to older people, nutrition is very important. Too little exercise, a lack of good proteins and the loss of muscle mass all impact on health. Overall, the quality of life can suffer a lot, which is an important issue for Martin Andermatt. After all, quality of life is an important issue for all people. Especially when they get older. Then you also need a good measure of discipline if you want to stay physically and mentally fit over a long period of time.
Just thinking that maybe you should lose some weight is not enough to really achieve that. Only then, when one becomes active in the process, will success be achieved. So it’s about real action, which is always crucial for change.
A first step for Martin Andermatt in his encounter with liver fasting was to pick up the HEPAFAST® preparation himself in Bern and not simply have it sent to him. In the Swiss1Chirurgie clinic, he had his measurements taken, so to speak. What really counts are actual and current values. Martin Andermatt already knows this from his sporting career.
Motivation counts
As in many other areas, the right motivation is the best starting point for good results in liver fasting. If one’s own motivation can then be supported in a discussion with a medical specialist, this is a good prerequisite for active action.
What counts then is the real doing. Not tomorrow or perhaps the day after tomorrow, but ideally right away, one should start with what one has recognised as good and right for oneself.
From Martin Andermatt’s point of view, it is sometimes the small vanities that can be an impetus for liver fasting. Who doesn’t want to please their partner even at an older age? Who doesn’t want to be active and fit even as they get older? You also want to be a role model for the children and if you are a coach, it all has something to do with a positive aura on the people you are training. Only if you like yourself can you radiate that positively, says Martin Andermatt.
In addition, of course, there are the thoughts about one’s own health. Even if you have paid absolute attention to a healthy diet and lifestyle for many years, sometimes this changes as you gain experience in life. However, personal health always remains the most important asset. You have to decide what is good and what is right. Those who decide for themselves do not have to let others decide for them. And health should always be a very important factor in these decisions as well.
What advice should you give to active athletes at the end of their career?
In general, active athletes eat a diet very rich in carbohydrates, as they need this energy for their physical exertion. Often, at the end of their career, it can be observed that many athletes quickly gain weight and even tend to become obese. Then it is important to get back to normal life as well. A deeply human factor also plays an important role here. As an athlete, you are suddenly no longer in demand. This can quickly lead to letting oneself go. In every respect. It is then all the more important to recognise one’s own human value. You have to see what you still want to achieve in life and what you can accomplish and with what charisma you want to meet your fellow human beings. The short-lived lucky charms like good food, Coke or a bag of crisps are then not really what you need. The short happiness is a fallacy that in the end only makes people dissatisfied and unhappy.
The recommendation for active athletes at the end of their career
In any case, those who are at the end of their career have to train off slowly. It is not the end from one day to the next that counts, but the gradual change to a normal status. Just as you then gradually say goodbye to high athletic performance, you naturally also have to change your diet. The mental load also changes, which must also be considered.
Martin Andermatt is convinced that what counts now are good conversations, even beyond one’s own horizon of experience. Good medical supervision can be useful. This is not about fear of any diagnosis, but about developing visions for one’s own future. At the same time, it is also important for Martin Andermatt to simply live in a more relaxed and happy way.
As a coach, he follows a very clear philosophy, which he likes to sum up in three words: Laugh, learn, sweat. When he passes this on to his players, Martin Andermatt himself also likes to think about whether he has already laughed, learned and maybe even sweated today. The most beautiful thing is when you can give the players something beyond pure sport that is still of value for life after active sport.
Your own experiences with liver fasting
From his own experience, Martin Andermatt can only associate liver fasting with pleasant perceptions. This includes above all the real feeling of well-being and the new energy he felt for himself.
Especially in times when one wants to recognise oneself anew, liver fasting is an additionally exciting experience. Martin Andermatt has already completed a liver fasting cure with HEPAFAST® three times and is sure that he will do it again and again. If only because of all the positive energy it has given him. He is also happy to recommend liver fasting to others. He stands behind it with all his personality and experience.
Of course, it can be difficult for individuals to face their issues. People often prefer to make fun of themselves instead of tackling important changes. Certainly also because change can be uncomfortable. But those who listen to themselves know that only change brings change. And that is exactly what applies to liver fasting.
The question is not why you fell into the water, but how you get out of it. It’s about making decisions and then following through with them consistently. And if you need support to do that, you have to get that support.
Belching, obesity and diabetes – recognising connections
At the 4th Helvetius Holding AG symposium, Dr. med. Jörg Zehetner, Professor (USC), dealt with the connection between reflux diseases, obesity and diabetes in a detailed lecture. In most cases, there are causal relationships between the different clinical pictures, which must also be taken into account in medical therapy. While a large proportion of overweight patients also complain of reflux, the links between obesity and diabetes are even more apparent. Both diseases are reciprocal consequences and triggers of the other disease. This also affects the professional approach to therapy. The full article on the lecture, a video stream of the lecture and further information can be found here.
In his highly acclaimed lecture at the 4th Helvetius Holding AG symposium at the Talent Campus Bodensee in Kreuzlingen, Dr. med. Jörg Zehetner, Professor (USC), revealed the connections between belching, obesity and diabetes. Based on the latest scientific findings and from his own medical clinic, Dr. med. Jörg Zehetner has developed a model from this that makes it clear how the connections are to be seen, which health restrictions and experiences result from this and which medical interventions are indicated.
Dr. med. Jörg Zehetner is considered THE specialist in visceral and obesity surgery in Switzerland. His comprehensive training and specialisation also make him a sought-after specialist abroad, for example as a supporting luminary to his professional colleagues in the United Arab Emirates. The extended training in the USA and his own scientific research have made Dr. med. Jörg Zehetner a proven specialist in his field. As the head of one of the largest private practices in Switzerland, he is the head of Swiss1Chirurgie and offers patients, their relatives and specialist colleagues a wide range of modern treatment methods and expanded options for therapy in the association of companies that operate under the umbrella of Helvetius Holding AG.
Individual clinical pictures, diagnoses and complaints are often closely linked and not infrequently form a kind of causal reaction chain in which one abnormality causes the other or is a consequence of previous illnesses. Therefore, it is important to look for and find the possible connections between different symptoms.
The clinics in the Helvetius Holding AG network
First, a few introductory words about Swiss1Chirurgie. The Swiss1Chirurgie is a visceral surgery clinic in which Dr. med. Steffen, Dr. med. Anita Scheiwiller, Dr. med. Metzger, Dr. med. Flückiger, Dr. med. Fringeli and Dr. med. Jörg Zehetner provide highly specialised medical services for patients. The Swiss1Chirurgie sites are in Bern, in Solothurn and in Valais, where patients are treated primarily in the specialties of bariatrics, reflux diseases, oesophageal and stomach cancer, colon, thyroid diseases, liver diseases and hernias.
The Centre for Bariatric Surgery ZfbC has established itself as a specialised pre- and post-operative care centre for bariatric surgery in conjunction with Swiss1Chirurgie. Here, patients are cared for holistically by the specialists before a necessary operation and after the surgical procedure.
The Gastroenterology Group Practice Bern GGP is the centre for endoscopic examinations and functional diagnostics. Chronic diseases of the gastrointestinal tract are also treated here.
An internal medicine clinic has established itself in the Bern PZBE clinic and offers services here not only in the field of internal medicine, but also in the special field of psychosomatics.
All specialist practices under the umbrella of Helvetius Holding AG are staffed with experienced medical specialists, work closely with each other and thus provide holistic and professional healthcare and necessary medical interventions in the overall concert of specialist medical services for the benefit of patients.
Reflux – Acid regurgitation
Everyone is certainly familiar with acid regurgitation, for example after a sumptuous and very fatty meal or after excessive alcohol consumption. An occasional belching with clearly defined temporary symptoms is not a problem at first.
Acid reflux only becomes a problem if it occurs chronically, i.e. more or less repeatedly, and if it is actually disturbing or even annoying to the body. Then we are talking about reflux. By reflux we mean that gastric juice rises from the stomach into the oesophagus. The stomach acid not only leads to the familiar unpleasant sour sensation, but in its chronic form can also lead to serious burns of the oesophagus and even to the development of oesophageal cancer.
The whole thing is referred to in medical parlance as Gastroesophageal Reflux Disease, or GERD for short, and is a serious disorder with disease value. This is a disease of the sphincter and/or diaphragm, but is favoured by other factors. One of the factors that cause gastric juice to be expelled into the oesophagus is a valve at the junction between the oesophagus and the stomach that does not function normally. Normally, this valve prevents acidic gastric juice from being pushed up into the oesophagus. If the function of this valve is disturbed, reflux can occur. This valve is located at the transition from the thorax to the abdominal cavity, which is practically formed by the diaphragm. The oesophagus runs through the diaphragm.
A normal function of the valve requires that this valve itself is organically completely without findings. Furthermore, a normal weight is a good prerequisite for the undisturbed functioning of the valve. If you are overweight, the increased pressure on the abdomen and diaphragm alone means that the function of the valve can be restricted. The mechanism works in such a way that the lungs pull in normal function, while an overfull abdomen pushes against it, so that the function of the valve is affected in only one direction, upwards. As a result, a defective or weak valve at the transition from the oesophagus to the stomach allows gastric juice to flow back.
It should be noted that the stomach does not only contain gastric acid. Pepsin, bile, pancreatic juice and of course food components in variously decomposed forms are found in the stomach. If the pumping function of the oesophagus is disturbed and the valve is not fully functional, all these components are pressed into the oesophagus, which is not only unpleasant but can also become really dangerous in the long term.
Treatment of reflux disease
Reflux can be treated conservatively in many cases. A change in lifestyle is just as helpful as a diet. Avoid spicy foods, coffee, greasy and fried foods, onions, garlic and tomatoes, fruits and fruit juices. Furthermore, dark chocolate with a high cocoa content, alcohol, carbonated drinks, large food portions and, in individual cases, certain medicines should be avoided.
Often, avoiding such factors already helps to reduce reflux. It is remarkable that smokers complain more about reflux, as smoking also has a loosening effect on the function of the valve described above. The same applies to other stimulants, which we have described here before with dark chocolate and alcohol.
When changing our lifestyle, the most important thing is that we don’t always eat the really big portions, but rather smaller portions more often. Opulent food right before going to bed should also be avoided. There are a number of medications that affect the function of the oesophago-gastric valve. A whole industry has grown up around acid reflux, which often sells its medicines without a prescription, virtually at discount stores.
The function of such medicines is usually only oriented towards the symptom, but not the cause. Such medicines do not stop the actual reflux, but reduce the production of stomach acid. They are nothing more than so-called acid blockers, but have no effect on the production of bile, pepsin or pancreatic juices and have no effect whatsoever on the defective or weakened valve at the junction between the oesophagus and the stomach. Therefore, the mode of action always remains limited and ultimately does not change the causes of reflux.
This means that only a part of the whole symptomatology, i.e. the stomach acid, is removed or reduced, but the problem as such remains.
Reflux surgery
Until ten years ago, only two procedures were actually established for reflux. On the one hand the Nissen fundoplication and on the other hand the Toupet fundoplication. While good oesophageal function is a prerequisite for the Nissen fundoplication, the Toupet fundoplication can also be used in cases of poor oesophageal function.
At Swiss1Chirurgie, we have been using the LINX system in the therapeutic treatment of reflux in Switzerland since 2015. In simple terms, this LINX system is a magnetic ring made up of individual parts on a kind of belt. This magnetic band closes the transition between the oesophagus and the stomach, but opens under a certain pressure so that, on the one hand, normal food intake into the stomach but, on the other hand, vomiting remains possible. However, the relatively light pressure of reflux is stopped so that no gastric juices can push up into the oesophagus.
Another advantage of this system is that a normal diet is possible postoperatively and air can also be expelled, which is not to be expected with the older procedures. Furthermore, when using the LINX system, there is significantly less of the feeling of fullness known from the other methods and no increased flatulence.
As part of a medical study, we have also been using RefluxStopTM in Swiss1Chirurgie since 2020. This involves fixing the stomach to the oesophagus in order to maintain the lower sphincter in the abdomen. A small silicone ball holds the prepared area in position, allowing an almost natural situation to be restored. In all such operations, the existing diaphragmatic hernia must also be treated surgically.
Jörg Zehetner, MD, is the only surgeon in Switzerland to offer his patients all of the procedures listed here. He always makes his decisions individually and on the basis of the situation found in the individual case. The important starting point for the decision is the function of the oesophagus. With normal oesophageal function, the LINX system and the Nissen fundoplication can be used well. In cases of moderately to severely reduced oesophageal function, the Toupet fundoplication, the RefluxStopTM system or, in exceptional cases, a Dor fundoplication are more likely to be used. In the clear majority of cases, the proven LINX system can be used.
Problems due to reflux
In addition to the actually already unpleasant appearance of reflux due to the repeated acid regurgitation, reflux also hides clearly dangerous constellations. The constant acid attack on the inner oesophagus often leads to infectious processes. These infections can lead to changes in the oesophageal mucosa. As a result, the mucous membrane changes in such a way that at some point it also shows tissue changes that are visually very reminiscent of stomach tissue. Such tissue then also has the potential to develop cancer. So oesophageal cancer cannot be ruled out and is always on the cards as it progresses. This is not something to be taken lightly. Adequate treatment is urgently needed.
The statistical evaluation shows that oesophageal cancers have increased significantly since 1975. Here, an increase of 700 percent can be observed in the last 30 to 40 years. For men, it is the cancer that has increased the most worldwide.
If we look at the correlations between reflux, obesity and diabetes in the following, some correlations become clear even in the statistical analysis.
Connection between overweight and reflux
In general, it can already be stated here that the probability of suffering from reflux increases significantly with the presence of severe overweight. For example, the body mass index BMI was compared and correlated with acid exposure. A BMI of 30 or more is referred to as obesity, which is expressed in various classifications. A BMI of 35 or more can be considered pathologically overweight.
Being morbidly overweight is not just a matter of external symptoms such as a colloquial “beer belly” and the inevitable fat deposits. With a BMI over 40, we already speak of a metabolic syndrome, which can be defined by diabetes, high blood pressure, elevated cholesterol levels, fatty liver, high blood fat levels as well as arthritis and gout.
These symptoms also increase the risk factors for cardiovascular disease, stroke, sleep apnoea, cancer, abdominal wall hernias and reflux disease. The risk of oesophageal cancer then increases again with the reflux diseases. This observation already shows that the connections and transitions between reflux, obesity and diabetes must be considered causally.
When assessing the development of obesity, the tendency is that obesity is increasingly observed worldwide, especially in the developed industrialised countries but even in the developing countries. And this is happening at a breathtaking rate of progression in close connection with a food oversupply with virtually unlimited availability of food.
As body weight increases, it is not only the outwardly visible fat deposits that occur. The liver is always particularly affected, which develops from a healthy liver to a fatty liver and even cirrhosis with increasing obesity. On the topic of fatty liver, we have provided a separate contribution and lecture by Dr. med. Michaela Neagu from the Gastroenterological Group Practice Bern GGP. A contribution and lecture by Dr. Hardy Walle on liver fasting is also available.
If you look at the phenomena of obesity with a close look at the metabolic processes in the body, then a concrete connection to diabetes can also be established. If you bring together the statistical data on obesity and diabetes, the interaction becomes more than clear.
It should also be clearly assessed that a fatty liver is often the cause of diabetes, but diabetes can also be the cause of a fatty liver. Here, a kind of vicious circle closes that can only be broken by appropriate medical interventions.
The function of the pancreas is clearly related to diabetes. The pancreas lies anatomically behind the stomach and fulfils two essential functions. On the one hand, it supports the digestive function, on the other hand, it produces insulin, which is required for the metabolisation of sugar, more precisely glucose. Insulin affects the sugar balance in the liver, fatty tissue and muscles. In overweight people, this metabolism is disturbed. The fatty cells show resistance to insulin uptake, which significantly disturbs the metabolisation of glucose. As a result, blood glucose levels deviate from normal. Progressive diabetes mellitus develops.
Diabetes mellitus is divided into two types. Type 1 with subgroups 1a and 1b. Diabetes mellitus type 1a is mostly observed as a congenital form in childhood and manifests after viral infections.
Type 1b is seen up to about 35 years of age and is associated with islet cell antibodies and autoimmune system disorders.
Diabetes mellitus type 2 used to be called adult-onset diabetes and occurs mainly in overweight people with a disturbed metabolism. In the meantime, we are increasingly observing diabetes mellitus type 2 also in children and adolescents who are very overweight. Type 2 diabetes mellitus is even more common in children and adolescents than type 1.
The problem with diabetes is not only the damaged metabolism. The blood vessels, liver and heart function are also affected. Arteriosclerosis often occurs, leading to narrowing or blockage of blood vessels. The risk of heart attack increases fivefold and the risk of stroke triples.
The course of diabetes is a progressive process that initially appears to be easily manageable, but as it progresses, it requires more and more specialist medical intervention. In the context of diabetes and obesity, it has been shown that surgically treated obesity patients often experience a better and faster improvement in diabetes than those with only drug treatment. Of course, if the obesity surgery is done after many years of an existing diabetes, the likelihood that the diabetes will also improve again is reduced.
Accordingly, it is important not to put off obesity surgery for a long time in patients with a BMI of 40 or more when diabetes is just beginning. The sooner action is taken, the greater the effects both on body weight and on preventing the progression of diabetes.
It is important to understand that obesity is a disease and must be treated as such. Different studies clearly show that in cases of severe obesity, obesity surgery is always the better solution compared to other medical interventions, also with an effect on diabetes.
Effects of metabolic surgery
If all experiences from metabolic surgery are considered in the context of reflux, obesity and diabetes mellitus, the following effects can be demonstrated in patients with a BMI over 40:
- generally improved quality of life
- greater improvement in blood glucose levels
- Reduced consumption of diabetes medication
- fewer vascular diseases
- fewer strokes
- reduced cancer risk
- Less overall mortality
- Higher weight loss than with conservative therapies
Only two to three percent of patients with a BMI over 40 achieve significant weight reduction in conservative therapies. Only patients with a BMI between 30 and 35 often show good results with conservative therapies.
View bariatric surgery as a whole
Bariatric surgery presents itself as a triad that does not stop at one surgical procedure. The operation alone does not solve the problem. Important is the interaction of
- Lifestyle change
- Change in dietary habits and
- surgical intervention with good pre- and aftercare
Modern surgical procedures have long since bid farewell to the gastric banding that has been used for many years. In the USA and Germany, the preferred outcome of the operation is the formation of a tube stomach. This affects up to 60 percent of patients. In Switzerland, the current level here is around 30 percent. Partial removal of the stomach also achieves hormonal effects, as the passage of food through the stomach is accelerated and the small intestine is much more likely to be activated with corresponding hormone release.
Another option is gastric bypass, which is performed laparoscopically. This technique is preferably used in patients with pre-existing diabetes or pre-existing reflux. With a share of about 70 per cent, this is the most frequently performed bariatric operation in Switzerland. A small gastric pouch is formed and connected directly to the small intestine.
Additional information
You can watch the entire lecture in its original wording, with additional questions and answers as well as interesting statistics here in the stream.
In addition, we recommend further articles and videos that were produced as part of the Helvetius Holding AG symposia.
Fatty liver and diabetes – the connections
In a lecture by the gastroenterological group practice GGP Bern AG (a company of Helvetius Holding AG), the gastroenterologist Dr. med. Michaela Neagu illustrates the connections between fatty liver and diabetes. Following the lecture, it becomes clear that fatty liver and diabetes form a vicious circle in which both diseases trigger and drive each other. In addition to diagnostics and the effects on overall health, the lecture also opens up a clear picture of how the course of the disease can be successfully influenced and, in the best case, reversed. We have made the lecture by Dr Michaela Neagu available in text form, but also as a video lecture and as a PowerPoint presentation. You can find out more here.
The experts at Helvetius Holding AG clarify
In a lecture by GGP Bern AG, Dr. med. Michaela Neagu presented the connections between fatty liver disease and diabetes mellitus. This is less about medical jargon and more about educating people about what a fatty liver is, what it means for people’s lives and whether there is a connection to diabetes mellitus.
Dr Michaela Neagu is a specialist in gastroenterology (gastrointestinal diseases) and general internal medicine in the Gastroenterology Group Practice Bern, a partner of Helvetius Holding AG, and has extensive experience and expertise in her specialist field.
In her lecture, Michaela Neagu, MD, highlights the clear connections between fatty liver and diabetes mellitus.
The fatty liver disease
Basically, a distinction is made between alcoholic fatty liver disease and non-alcoholic (metabolic) fatty liver disease. As the different names suggest, one form of fatty liver disease is related to excessive alcohol consumption, the other has nothing to do with alcohol consumption. In addition, there are manifestations such as viral liver diseases, autoimmune diseases, iron storage disorders and other conditions that promote fatty liver disease or make it possible in the first place.
Worldwide, about 25 percent of the population is affected by fatty liver disease. This makes fatty liver the most common liver disease of all. Among diabetics themselves, about 30 to 40 percent have a fatty liver. Also, about half of patients with severe dyslipidemia suffer from fatty liver disease.
How does a fatty liver develop?
A fatty liver occurs when the capacity of the liver cells to absorb fat is exceeded. This causes fat to be deposited in the liver itself, which can no longer be broken down by the liver. The accumulation of fat in the liver cells causes these cells to become inflamed and then send out messenger substances that inhibit the supply of insulin to the liver. Eventually, a kind of insulin resistance develops, so that insulin cannot work in the body as nature intended.
As a result, hyperglycaemia occurs in the body. This sends out a stimulus that causes even more insulin to be produced. The increased insulin level then further leads to increased fat absorption, fat synthesis and fat storage as well. This creates a cycle of action that deposits more and more fat in the liver, but also generally increases fat storage in the body far beyond normal levels.
What do people affected by fatty liver notice?
It is sobering to note that about half of all those affected live practically asymptomatic and accordingly do not worry at all about their liver health, for example. On the one hand, this may have a calming effect, but on the other hand, it is an alarm signal that effective therapeutic interventions only start late, usually very late.
Some patients experience general but rather non-specific fatigue. A certain faintness and perhaps once undifferentiated slight pain in the upper abdomen indicate that a serious condition could be present here. Mostly, however, this is not taken seriously by the patients themselves.
As a result, in most cases the fatty liver remains an incidental finding that only comes to light during the treatment of other diseases. This could be, for example, elevated liver values during a health check or visible changes in the liver during a standard ultrasound examination.
In general, there is a risk that untreated fatty liver can progress to cirrhosis. At the latest then, those affected realise that their liver is sick. Typical signs are then the well-known large water belly, certain bypass circuits in the organism and other signs come very late, however. In practice, everything is possible with the clinical picture of fatty liver, from no symptoms to severe and dangerous courses of the disease.
Between 50 and 90 percent of people with fatty liver are obese, i.e. clearly overweight. Signs of a metabolic syndrome are recognisable.
How can a fatty liver be diagnosed with certainty?
A few years ago, biopsy was the method of choice when the condition of the liver cells needed to be determined more precisely. To do this, a needle is inserted directly into the organ and a small tissue sample is taken. This tissue sample can then be further examined for fatty liver cells.
Thanks to advances in medical technology, we can now diagnose fatty liver without a biopsy in 90 percent of cases. With different imaging methods such as ultrasound or computer tomography, absolutely painless examinations can be carried out today without interfering with the body. Thanks to the excellent presentation, the fat content in the liver can be determined comparatively well with reliable values.
The basis for the evaluation of the ultrasound examinations is, for example, a comparison of liver and kidney tissue. If both organs are healthy, they have approximately the same structure and colour in the image. If the kidney tissue appears darker than that of the liver, then the lighter parts in the liver indicate fat deposits. In this way, a fatty liver can already be recognised with a fairly high degree of certainty.
If the specialists then decide to take a tissue sample, usually to exclude or detect additional liver diseases, the differences become even clearer. A healthy liver consists of neatly arranged and clearly differentiated cells. In fatty liver, the disturbance of the cell architecture due to the fatty deposits is clearly visible. This becomes even more obvious in the case of a pronounced fatty liver with infected cells.
What is the path to fatty liver
From a healthy liver to a fatty liver always takes time and certain circumstances. Various unfavourable factors cause fat storage in the liver cells, which can then further lead to infection in the liver itself. It doesn’t have to be, but it can be. However, when such an infection takes place, a certain remodelling in the connective tissue is driven forward, which can lead to complete scarring of the liver if left untreated. Then the stage of liver cirrhosis has already been reached. Liver cirrhosis, in turn, is a favourable factor for the development of liver cancer. This applies to about two percent of those affected. But even when liver cirrhosis has not yet been diagnosed, more and more cases of liver cancer in fatty liver are becoming known. And in the USA, fatty liver is now considered the most common reason for liver transplantation.
A look at diabetes mellitus
Usually we are talking about diabetes here. This is diagnosed when chronically elevated sugar levels are found in the blood. The body is over-sugared, so to speak. The factors that cause high blood glucose levels are a reduction in the effect of insulin and, in the course of time, often an insulin deficiency.
Currently, about six percent of the world’s population, including children, are affected by diabetes. In children, type 1 diabetes is mostly observed. With the increase in morbid obesity, also in children, type 2 is also becoming more common. Diabetes can be diagnosed in a very reliable and uncomplicated way in various test procedures.
What does diabetes mellitus mean for people’s lives?
The presence of diabetes mellitus is actually associated with serious risks and consequences for the health and life of those affected. One problem is the damage to the small veins. This mainly affects the kidneys, the retina of the eye and the nervous system. The range extends from relatively mild kidney problems to complete kidney failure requiring dialysis. In the case of retinal diseases, such disorders can lead to blindness due to diabetes mellitus. In terms of damage to the nervous system, there is a loss of certain sensory impressions, which can manifest itself, for example, in patients no longer being able to feel the ground beneath their feet. Problems with coordination and spatial position change are also observed. Gastrointestinal disorders with diarrhoea and other symptoms are also reported. Cardiac arrhythmias can complete the picture.
In addition to damage to the small veins, damage to the large veins is also a consequence of diabetes mellitus. Particularly worth mentioning here are coronary heart diseases. At least here, the risk of diabetes patients is significantly higher compared to the normal population. For diabetics, this risk can be assessed as about twice as high. A full 75 percent of diabetics die from a cardiovascular event.
The risk of suffering a stroke is also about 2.5 times higher than in the comparison group of people without diabetes. A circulatory disorder, especially in the legs, has a risk of 4.5 times more than in the comparison group. The diabetic foot is well known, which is caused by precisely these circulatory disorders and can even lead to the necessary amputation.
Diabetes mellitus also generally increases the risk of infection in relation to practically all infectious diseases.
The relationship of fatty liver and diabetes mellitus
What is special about the relationship between fatty liver disease and diabetes mellitus is the fact that both diseases can be mutual and reciprocal triggers as well as consequences of the other disease. This means: fatty liver patients are or often become diabetics and diabetics often suffer from fatty liver. So there is a causal relationship between fatty liver and diabetes.
Let us imagine a possible course of events: An initially physically completely healthy and normal person begins to gain weight for various reasons. Fat tissue increases and at some point the ability to store fat is exhausted. This then leads to a veritable flooding of the entire organism with free fatty acids. At some point, the organism becomes resistant to the effect of insulin and hyperglycaemia occurs. Now the question arises: Where to put the sugar?
Some of the free fatty acids are deposited in the liver cells, where they lead to the fatty liver already described. This significantly limits the liver’s ability to metabolise healthy fats. In addition, there is an increasingly pronounced insulin residual tendency, which in turn affects blood sugar in the interaction and ultimately leads to type 2 diabetes. Other effects are always included here, such as high blood pressure, disorders of the function of the pancreas, etc.
The mutual condition of fatty liver and diabetes creates a vicious circle that is difficult to break, and then only with radical methodology.
What can be done?
At least up to a body mass index BMI of 30, maximum 35, it is still possible to take countermeasures and something should be done actively. It is worth noting that the fatty liver is reversible, i.e. it can also be regressed. Even if liver infection has already occurred, the process can still be reversed. Timely action is crucial. If cirrhosis of the liver has already occurred, it can hardly be stopped. Nevertheless, even then, consistent lifestyle adjustments and regular check-ups should be aimed at preventing further liver damage.
The way back to a healthy liver is always through a reduction in body weight and a corresponding reduction in the over-fatness of the organism. Even a five percent reduction in body weight leads to a relevant defatting of the liver.
With seven to ten percent weight loss, infections in the liver or incipient scarring of the liver tissue can also be reversed. These are encouraging facts that have been sufficiently tested and researched.
Several factors are crucial for weight loss. This starts with a significant reduction in calorie intake and continues with healthy and regular exercise. A period of at least eight weeks, but usually considerably more, is to be set. The closest possible consultation and care by specialists is highly advisable, as other risk factors must also be observed and ruled out. This applies especially to cardiovascular risks.
Toxic foods such as alcohol, drinks with a high fructose content and nicotine should be avoided at all costs.
You can watch the entire lecture by Dr. med. Michaela Neagu with a lot of additional interesting information and further questions and answers here in the video lecture.
A PowerPoint presentation on the topic illustrates and complements the lecture.



