Morbid obesity is a chronic disease
After London 2017 and Dubai 2018, the World Congress of the International Federation of Societies of Obesity Surgery (IFSO) was held this year in the Spanish capital Madrid.
One of the topics was the stigmatisation of overweight patients. There was agreement on this topic that morbid obesity is indeed a chronic disease and requires appropriate treatment. The times when overweight patients are ridiculed, laughed at or even insulted in public must finally be over. With obesity surgery, this group of patients also has access to a variety of different treatments and interventions that can successfully address and permanently treat this condition.
This was an important topic in the meeting of bariatric surgery specialists from the cantons of Switzerland, who had the opportunity to exchange views on this topic at a joint dinner during the congress.
What is the state of facts?
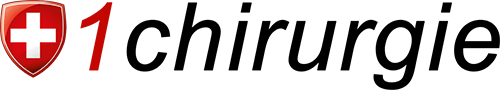
In Switzerland, there are primary centres and centres of reference for obesity surgery. Whereas in a primary centre only the first operation for patients with BMI 35-49 may be performed, in a reference centre re-operations (new corrective operations) and very heavy patients (BMI greater than 50) may be operated on. This is an arrangement that makes it difficult for many patients to undergo continuous treatment that is ultimately accompanied by visible, tangible and countable success in the long run.
Swiss1Chirurgie has responded to this together with the Beau-Site clinic in Bern and the Espace Chirurgie clinic in Biel. The obesity surgeons in Biel perform the initial operations at the Hirslanden Klinik Linde and the re-operations with Dr Zehetner at the Klinik Beau-Site. At the Beau-Site Clinic in Bern alone, 500 of the 4,500 surgical procedures performed annually throughout Switzerland are carried out. At the Centre for Bariatric Surgery in Bern (ZFBC), these patients are pre-cared for, operated on by Swiss1Chirurgie surgeons and then followed up again at the ZFBC. This means that within the Hirslanden network, Swiss1chirurgie has the greatest expertise in bariatric surgery in Switzerland and guarantees the highest level of patient safety.
What patients with problems after obesity surgery can do
Have you already had obesity surgery and are not receiving follow-up care? Or have you put on a massive amount of weight again after the operation and don’t know what to do next?
Ask your general practitioner to refer you to one of our Swiss1Chirurgie locations in Bern, Solothurn or Brig (www.swiss1chirurgie.ch). We can then admit you to our aftercare programme at the Centre for Bariatric Surgery (www.zfbc.ch) or arrange for clarifying examinations for a possible corrective operation to lose weight again.
Of course, the World Congress also focused on the big issues in obesity surgery. Here are a few key points on the results:
- The most common obesity surgery worldwide is the tube stomach (sleeve).
- The gastric band is hardly ever done anymore, under 1% of all overweight operations.
- In patients with reflux, the gastric bypass has advantages over the sleeve.
- In severely overweight patients, OAGB (one loop anastomosis gastric bypass) is also a possible option.
- Endoscopic revisions such as anastomotic stenosis with Apollo Overstitch are used more frequently, especially in cases of dumping and recent weight gain.
Learn more? Then simply contact me and let me advise you on the most promising options for the surgical treatment of obesity and reflux disease.